
Author: Bob Brensel | President, Pharmacist | ScriptWorks
Bob Brensel, RPh, earned his Pharmacy Degree at University of the Pacific in Stockton, California in 1980. Former California Pharmacists Association’s Award Winner for Recognition of Outstanding Achievement in Compounding Pharmacy. Read More →
When Menopause Feels Like It Took Over Your Life
You’re a California woman navigating menopause. Maybe you’ve gone through hot flashes, night sweats, mood shifts, and sleep disruptions. But above all, some of the most distressing symptoms may be creeping in slowly: a persistent fatigue you can’t shake, a decline in motivation, a dwindling interest in intimacy.
You might feel like your body isn’t you anymore. The simplest things that used to energize you — a morning walk, an afternoon project, connecting with your partner — now feel like uphill battles. Daily life, relationships, work — everything feels subtly “off.”
If you’re in that place, you’re not alone — and there may be options beyond standard hormone therapy. One such option increasingly discussed is topical testosterone (a compounded cream) at a low dose (for instance, 2 mg/mL). Let’s explore what that means, where the evidence stands, and how a careful practitioner might consider it in practice.

Statistics and Facts About Menopause
| Topic | Summary | Details |
|---|---|---|
| Age & Onset | Natural menopause 45–55, premature <40 | Most women experience natural menopause between 45–55. Premature menopause can occur before age 40 due to chromosomal, autoimmune, or unknown causes. |
| Duration | Perimenopause lasts several years | It begins with cycle changes and ends one year after the final period. |
| Population | 26% of women 50+ globally | This is up from 22% a decade earlier, and the number is increasing. |
| Longevity | Life expectancy at 60: 21 more years | Menopause care supports healthy aging and long-term wellness. |
| Symptoms | Hot flashes, night sweats, insomnia, mood changes | Symptoms vary; some are mild, others affect quality of life for years. |
| Bone Health | Reduced bone density | Loss of estrogen after menopause significantly increases the risk of osteoporosis and fractures. |
| Heart Health | Increased cardiovascular risk | Women’s natural advantage over men diminishes after estrogen levels drop. |
| Sexual Health | Vaginal dryness, pain during sex, incontinence | Thinner vaginal walls can increase risk of STIs including HIV. Incontinence may also occur. |
| Reproductive Health | Pregnancy still possible during perimenopause | Providers recommend contraception until 12 consecutive months without menstruation. |
| Public Health | Menopause care often missing | Many women are unaware of symptom management options, and many providers are untrained. |
Source: WHO
Why Testosterone for Women?
The role testosterone plays in women
- Testosterone isn’t just a male hormone. In women, it supports libido, sexual arousal, energy metabolism, mood, muscle strength, and bone health (to a degree).
- During and after menopause, total and free testosterone levels tend to decline, which may exacerbate symptoms like low energy or reduced sexual desire.
- Many randomized controlled trials (RCTs) of testosterone in women use non‑oral routes (e.g., gels, patches, creams) because they avoid first-pass liver metabolism and may carry fewer risks for lipids or systemic peaks.
Evidence so far
- In women with hypoactive sexual desire disorder (HSDD), adding transdermal testosterone (patch, gel, cream) to estrogen (or, in some trials, even alone) has been shown to increase the number of “satisfying sexual episodes” compared to placebo.
- Meta‑analyses and reviews point toward modest benefit for sexual function, but emphasize “non-oral” delivery for improved safety profiles.
- In one landmark RCT (the INTIMATE NM1 trial), 814 postmenopausal women with HSDD (not on estrogen) were randomized to a testosterone patch delivering 150 or 300 micrograms/day vs placebo. At 24 weeks, the 300-µg group had a mean increase of 2.1 satisfying sexual episodes per 4 weeks vs 0.7 in placebo (p < .001) — though androgenic side effects (hair growth) were more common.
- The global consensus on testosterone therapy for women highlights potential benefits.
Topical vs other delivery routes
A low‑dose topical cream (e.g., 2 mg/gm) is attractive because:
- It can be titrated more flexibly (dose up or down).
- It avoids spikes in systemic levels seen with injections or high-dose oral formulations.
- The skin acts as a “reservoir,” enabling slow absorption.
- It’s potentially more convenient and less invasive.
However, dosage consistency, absorption variability (skin thickness, site, hydration), and transfer risk (to others via skin contact) are important practical challenges.
2-mg/gm Topical Testosterone Cream — What That Means in Practice
- Concentration of testosterone in the cream base is 2 mg per mL of cream.
- Physician would monitor serum total and free testosterone, sex hormone binding globulin (SHBG), liver function, lipids, and clinical symptoms over time.
- Goal is to reach mid-physiologic premenopausal female testosterone levels (not the male range).
- Application guidelines — such as applying to clean, dry skin (inner forearm or thigh), avoiding contact with others until fully absorbed, and rotating sites — matter for safety and consistency.
In summary: 2 mg/gm is a “starting vehicle” in the compounding lab; the actual therapeutic dose is determined by the prescriber and the patient’s individual absorption and response.

Example Scenarios: When a Doctor Might Consider Compounded BHRT Topical Testosterone Cream
Here are illustrative scenarios (hypothetical) in which a well-informed practitioner might consider prescribing compounded BHRT, including a low-dose topical testosterone component.
| Scenario | Clinical Context & Rationale | Monitoring & Precautions |
|---|---|---|
| “Marisol, 52” | Marisol is in early menopause. She’s on estrogen + progesterone therapy. Her hot flashes and night sweats are well-controlled, but in the past year, she’s noticed crushing fatigue, low motivation, and a nearly absent libido. Lab testing shows low-normal total testosterone and somewhat elevated SHBG. After ruling out thyroid, anemia, depression, etc., her doctor suggests a low-dose compounded testosterone cream (e.g., 2 mg/mL, starting at 0.1 mL daily). Over 8–12 weeks, she reports improved “push” to get through the day, slightly more sexual interest. | Monitor testosterone levels (total, free), SHBG, liver enzymes, lipids every ~3–6 months; monitor for androgenic side effects; adjust dose as needed or discontinue if no benefit. |
| “Carmen, 60 (surgically menopausal)” | Carmen underwent oophorectomy a decade ago. She’s been on estrogen/progesterone but still reports low energy, brain fog, and poor recovery from exercise. Her doctor considers adding a low-dose testosterone cream to augment her overall hormonal balance and musculoskeletal support, especially since she desires an alternative to injections. | Start low, with careful discussion of risks and benefits. Monitor bone density, muscle strength, cardiovascular markers, and androgenic side effects (voice change, hair, etc.). Reassess in 6 months. |
| “Lucia, 55, estrogen-intolerant” | Lucia has a contraindication or intolerance to estrogen therapy (e.g., history of certain estrogen-sensitive conditions). She presents with symptoms suggestive of androgen deficiency (low libido, low energy). Her provider may consider whether a compounded testosterone cream (without estrogen) could offer symptom relief. | This approach is more speculative because evidence is less robust, and careful screening is vital (breast health, cardiovascular risk, lipids). The clinician would proceed only after informed consent and in close follow-up. |
| “Ana, 57, partial responder to standard HRT” | Ana is already on a standard FDA-approved estrogen + progestogen regimen, but still reports suboptimal improvement in energy, drive, and mood. The doctor may add a small amount of compounded testosterone (2 mg/mL cream) as a fine-tuning adjunct, essentially a “top-up” to her regimen. | Because combination therapy complexity increases, monitoring becomes more important: hormone levels, metabolic panel, side effects, and reconsidering discontinuation if benefits plateau or risks emerge. |
In every scenario, the decision should involve shared decision-making and careful monitoring over time.
Potential Benefits of Topical Testosterone Cream for Menopausal Symptoms
Topical Testosterone Cream may:
- Help restore energy, motivation, and a general sense of well-being.
- Improve sexual desire, arousal, and satisfaction (especially in HSDD).
- Help support lean muscle mass or mitigate muscle loss in aging.
- Be a convenient and customizable route of administration (topical).
Topical Testosterone Cream may:
- Help restore energy, motivation, and a general sense of well-being.
- Improve sexual desire, arousal, and satisfaction (especially in HSDD).
- Help support lean muscle mass or mitigate muscle loss in aging.
- Be a convenient and customizable route of administration (topical).
Practical Safety Strategies
- Begin with a low dose and titrate up carefully.
- Monitor laboratory values regularly: total/free testosterone, SHBG, liver enzymes, lipids.
- Assess clinical response (energy, libido, side effects).
- Rotate application sites, avoid broken skin.
- Advise patients to cover the area once absorbed or wash hands, avoid skin contact with others.
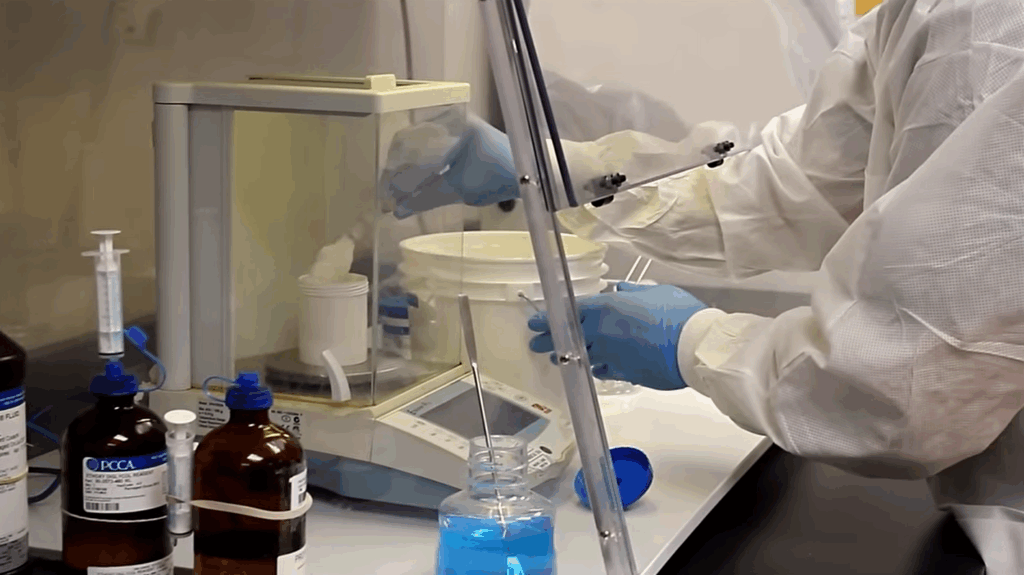
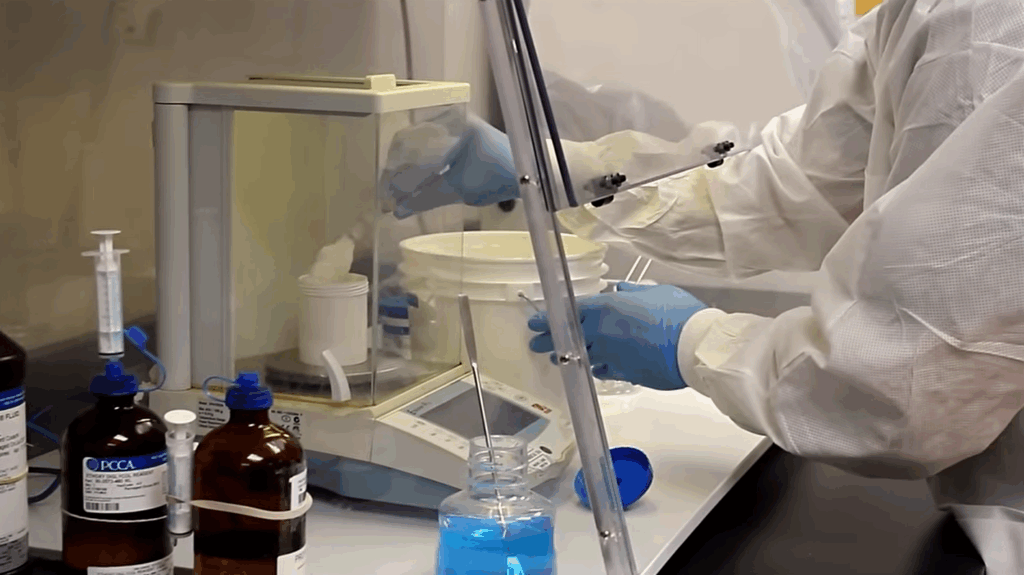
Use only from reputable compounding pharmacies with documented quality controls — aka, ScriptWorks!
Final Thoughts: Compounded Testosterone in California
For California women whose menopausal symptoms — especially low energy and low sexual desire — are profoundly disruptive, a topical compounded testosterone cream (e.g., 2 mg/gm) represents a possibility worth discussing with a clinician.
Compounding allows customized dosing, flexible titration, and patient-specific formulations, which is appealing when no FDA‑approved alternative exists for this indication. That said, both patient and provider must remain vigilant: start low, monitor frequently, and re-evaluate continuously.
References
Davis, S. R., Moreau, M., Kroll, R., Bouchard, C., Panay, N., Gass, M., Braunstein, G., Hirschberg, A. L., et al. (2008). Testosterone for low libido in postmenopausal women not taking estrogen. New England Journal of Medicine, 359(19), 2005–2017. Link
Glaser, R., York, A. E., Dimitrakakis, C. (2011). Beneficial effects of testosterone therapy in women measured by the validated Menopause Rating Scale (MRS). Maturitas, 68(4), 355–361. Link
Global Consensus Position Statement on the use of testosterone therapy for women. (2019). Maturitas. Link
Is testosterone important for women as they age? (2017). Maturitas. Link
Safety of testosterone use in women: a randomized placebo‑controlled trial of a testosterone patch. (2009). Maturitas. Link
Study of adverse outcomes in women using testosterone therapy. (2008). Maturitas. Link
- Sood, R., Warndahl, R. A., Schroeder, D. R., Singh, R. J., Rhodes, D. J., Wahner-Roedler, D., Bahn, R. S., & Shuster, L. T. (2013). Bioidentical compounded hormones: A pharmacokinetic evaluation in a randomized clinical trial. Maturitas, 74(4), 375–382. Link

